A major international clinical trial, known as the HARVEST trial, has found that giving a higher dose of rifampicin does not improve survival in adults with tuberculous meningitis, the most severe and deadly form of tuberculosis.
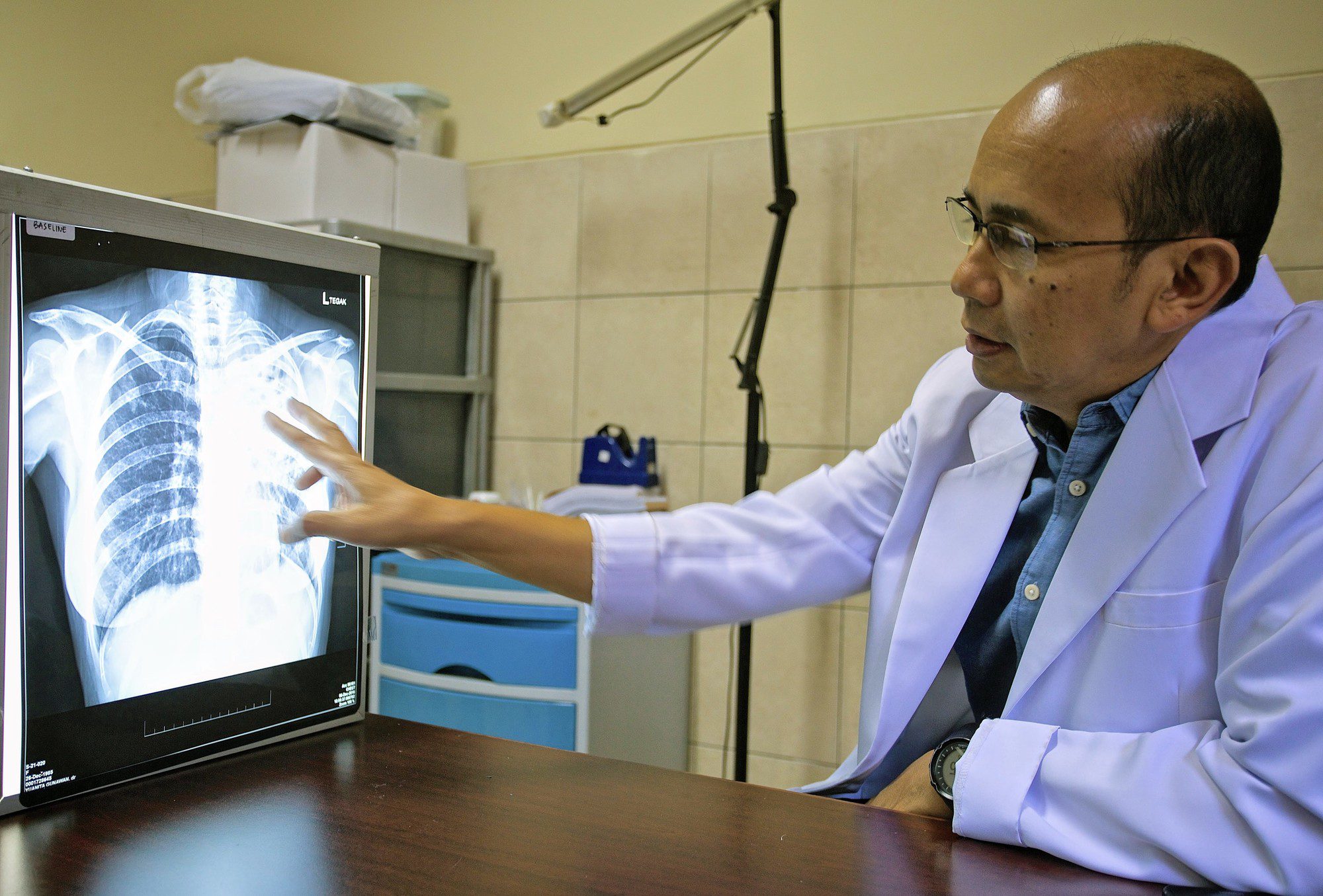
Tuberculous meningitis affects the brain and spinal cord and remains extremely difficult to treat. Up to half of patients die despite treatment, and many survivors are left with permanent neurological disability. One reason outcomes remain poor is that several standard TB drugs do not penetrate the brain well.
The trial published last week in the New England Journal of Medicine found that patients who received a 3.5-fold higher than standard dose of rifampicin were not more likely to survive than those given the standard dose.

After six months of follow-up, 44.6 percent in the high-dose rifampicin group had died, compared with 40.7 percent in the standard-dose group, a difference that was not statistically significant. Patients receiving the higher dose also recovered consciousness more slowly, and no improvement was seen in disability or longer-term neurological outcomes.
For more than a decade, researchers have explored whether increasing the dose of rifampicin could improve outcomes. Earlier, smaller studies in Indonesia, South Africa, and Uganda showed that higher doses could safely raise drug levels in the blood and spinal fluid.
The HARVEST trial was designed to test whether this strategy could translate into better survival, and is the largest and most rigorous evaluation to date of intensified rifampicin therapy for TB meningitis.
The trial enrolled 499 adults with tuberculous meningitis across nine hospitals in Indonesia, South Africa, and Uganda. Around 60 percent of participants were living with HIV, and most had severe disease at the time of enrolment.
Patients were randomly assigned to receive either a high dose of rifampicin (35 mg per kilogram per day), or the standard dose (10 mg per kilogram per day) during the first eight weeks of treatment. All patients also received other standard TB drugs and corticosteroids.
Researchers believe the worse early outcomes may be linked to an excessive inflammatory response in the brain when TB bacteria are killed more rapidly. In tuberculous meningitis, inflammation itself can be life-threatening and may outweigh any potential benefit of higher antibiotic drug exposure.
In Indonesia, the trial was conducted at Hasan Sadikin, Cibabat, and Immanuel Hospitals in Bandung, as well as in Dr. Cipto Mangunkusumo and the Indonesia Police Hospitals in Jakarta. It involved researchers from the Faculty of Medicine Universitas Indonesia and the Faculty of Medicine Universitas Padjadjaran.
“The findings provide essential direction for the global TB research community,” said Dr Darma Imran, a neurologist and Principal Investigator at Cipto Mangunkusumo Hospital and a researcher at the Faculty of Medicine Universitas Indonesia. “These results help doctors avoid treatments that add risk without benefit, and they add to the evidence needed to improve care for patients with tuberculous meningitis.”
“This trial is also a win for Indonesia,” said Prof Raph Hamers, one of the trial investigators based at OUCRU Indonesia. “Despite the disappointing clinical outcome, HARVEST demonstrates that complex, rigorous randomised clinical trials can be successfully conducted here, through collaboration with international partners. We hope that this trial will galvanize renewed global attention for this neglected, highly fatal disease, exploring strengthened anti-inflammatory treatments, more sensitive diagnostics, enabling earlier intervention, and enhanced supportive care.”
The researchers stress that these findings apply specifically to tuberculous meningitis and should not be generalised to pulmonary TB or other forms of tuberculosis, where drug penetration and immune responses are very different.
The study was led by Professor David Meya of the Infectious Diseases Institute, Makerere University in Uganda, and Professor Rovina Ruslami of Universitas Padjadjaran in Bandung, Indonesia. Other collaborators were from Radboud University Medical Center in the Netherlands and the University of Minnesota in the United States. The trial was funded by the UK Medical Research Council through the Joint Global Health Trials scheme.